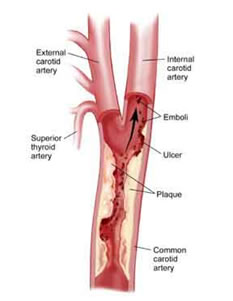
Carotid artery disease is the most common cause of stroke, which remains one of the most disabling conditions in our society. Many strokes could be avoided with early recognition and treatment of carotid artery disease. Atherosclerosis, the disease that affects our heart arteries and causes heart attack, is the same pathology that affects the carotid arteries. Build up of atherosclerotic “plaque” in the carotid arteries in the neck leads to the possibility of small bits of the plaque breaking off (emboli) and travelling with the blood flow to the small arteries in the brain, blocking these arteries and thereby causing a stroke (death of that part of the brain supplied by the blocked artery).
What are the risk factors?
The most common risk factors include:
- High Blood Pressure (Hypertension)
- Smoking
- Diabetes
- High Cholesterol
- Personal history of heart disease or other vascular disease
- Family history of cardiovascular disease (especially heart attack, stroke)
These are the same risk factors that result in the formation of atherosclerotic plaque/ hardening of the arteries throughout the arteries in the body.
It is important as part of the management of carotid artery disease to optimise these risk factors to prevent progression of plaque formation.
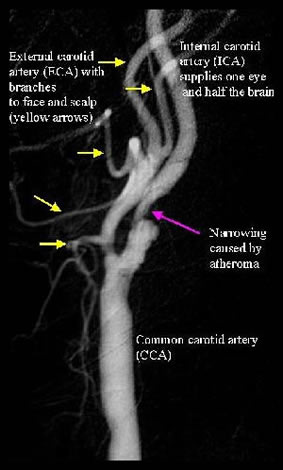
Carotid Artery Anatomy
What are the symptoms?
Disease in the carotid artery may be silent (asymptomatic), or can result in symptoms of a transient ischaemic attack (TIA) or a stroke.
TIA (also known as a “mini” stroke) is a condition that resolves within 24 hours. It means that you are at increased risk of a more major stroke in the near future. Some patients are lucky enough to have these “warning” attacks, though the symptoms (see below) are too often ignored as they may resolve very quickly. A stroke results in a permanent neurological deficit. Unfortunately, a stroke may be the first presentation of carotid artery disease.
Symptoms (for both TIA and stroke) include:
- Visual disturbances (usually in one eye, called amaurosis fugax, typically involving a short period of loss of vision in the affected eye, determined by covering each eye individually to check that only one eye is involved)
- Speech difficulties (the most common being an inability to be able to find the correct words, whilst understanding what other people are saying to you, called “expressive dysphasia”)
- Difficulty moving or weakness / clumsiness in an arm or a leg or both on one side of the body
- Altered sensation on one side of your body
Diagnosis
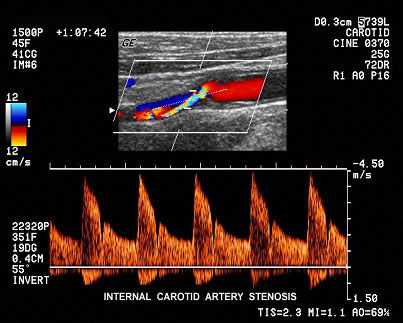
The first part of diagnosis is to recognise either those at risk or the warning symptoms (TIAs above). Those most at risk include males over 55 years of age, history of previous smoking, known heart disease, high blood pressure, diabetes, high cholesterol, family history of heart attack or stroke. Patients with any of these risk factors should be considered for “screening” of their carotid arteries which can be done simply and non-invasively with good vascular ultrasound. This provides an accurate estimation of the degree of narrowing caused by the plaque. The severity of narrowing is directly related to the risk of stroke. If more information is required, CT scanning or Magnetic Resonance Imaging (MRI) can be performed, though is rarely required.
What are the treatment options?
Treatment options for carotid artery disease will depend on the severity of stenosis (narrowing) of the artery, whether the patient is symptomatic or asymptomatic and general health or other conditions affecting the patient. All patients identified with carotid artery disease (or with risk factors for atherosclerotic disease in general) should be treated with control of these risk factors. In particular, control of blood pressure and diabetes, smoking cessation, control of cholesterol and blood “thinning” agents such as low dose aspirin therapy if no contra-indication exists. Specific treatment for carotid artery disease includes surgery (carotid endarterectomy, CEA) or carotid artery stenting (CAS).
Carotid Endarterectomy:This is an operation that involves removing the plaque from the artery thus preventing further debris travelling to the brain. It can be performed under local or general anaesthetic. Whilst general anaesthetic is probably more common, there is a growing trend to performing the surgery under local anaesthetic around the world. Our practice has been performing the surgery under local anaesthetic (with some sedation) for many years with a belief that this is lower risk for the patient. After removing the plaque from the artery, the artery is repaired by sewing a synthetic patch to the artery to minimise the risk of further narrowing the artery. Hospital stay is usually short at 1 or 2 nights with relatively quick recovery times for most patients.

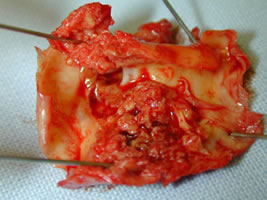
CEA, showing plaque removal and closure of the artery with a synthetic patch with removed soft and friable plaque
Carotid Artery Stenting: In this procedure, a stent is placed over the plaque within the artery thereby stabilising it, rather than removing it. This is performed through a small puncture in the groin as for any angiogram. Hospital stay is similar to surgery (1 or 2 nights). Whilst it sounds simpler than surgery, carotid artery stenting is not without some risk.
The advantages and disadvantages of both of these procedures (CEA and CAS) can be discussed during consultation. Remember that as vascular surgeons, we are able to offer non-biased advice on BOTH of these procedures, both of which are performed by us, as opposed to non surgeons who can only offer non-surgical treatment.”Minimally Invasive” treatment always sounds more attractive but may not always be the best or safest option for every patient. We are able to tailor the most appropriate treatment plan to the individual patient.
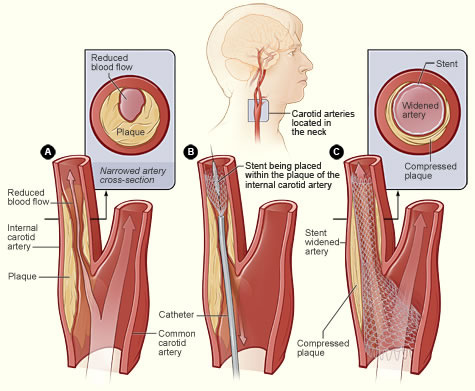
Carotid Artery Stenting