What are the management options?
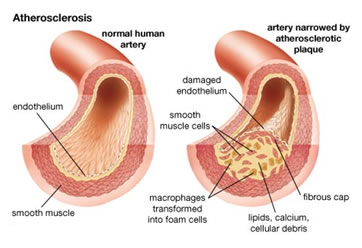
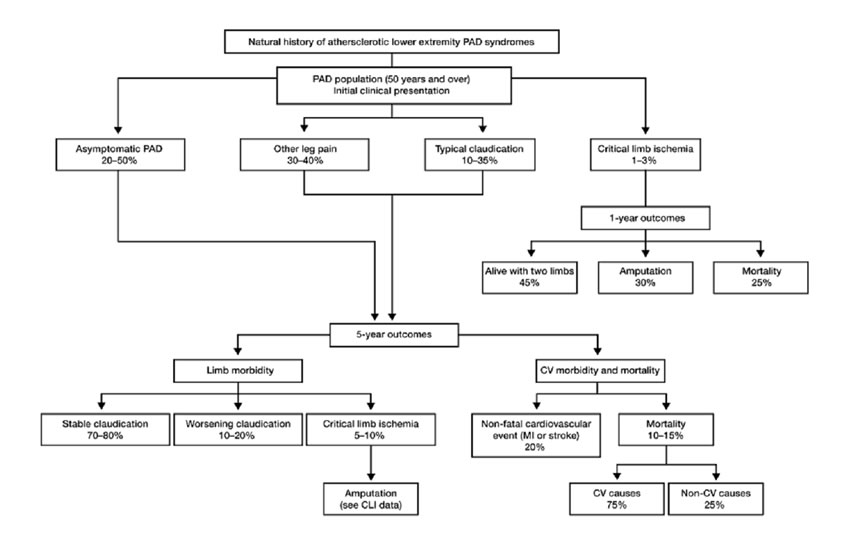
The management of patients with peripheral vascular disease needs to be directed at their overall atherosclerotic risk factors as well as consideration of revascularisation. The medical optimisation of risk factors is important. Advice and help in regards to ceasing smoking, good blood pressure control, good glucose (“sugar”) control for diabetics and cholesterol lowering measures is essential. All patients should be commenced on a blood thinning agent (anti-platelet agent) such as low dose aspirin, unless contra-indicated. All patients should be considered for commencing on a “statin” agent to lower cholesterol regardless of their cholesterol levels unless contraindications exist. For many people, claudication can be managed conservatively with the above “medical” management, exercise (which can improve the walking distance for many people), learning to live and adapt to any limitation in activity (eg allowing more time to walk from one place to another with short “rests” as needed) and reassurance of the generally benign nature and natural history of this problem. Many people are walking around with complete blockages in the arteries in their legs without even knowing it!! For claudication, the need for intervention is really determined by the level of inconvenience for the patient.
If claudication is becoming disabling, there is rest pain or ulcers and/or gangrene, revascularisation is considered. Revascularisation may involve open surgery (bypass, endarterectomy) endovascular techniques (minimally invasive – balloon angioplasty, stents) or a combination of both. There are many considerations in order to provide the best revascularisation option for you. Most patients today are thankfully able to be offered some form of minimally invasive treatment for their PVD. Early assessment is recommended as treatment can become harder and more risky if the situation is allowed to progress unmonitored for too long. In some cases, treatment in the form of revascularisation is just not possible and in dire circumstances amputation becomes the only option. With modern endovascular and surgical techniques, this is thankfully becoming a much less common (and potentially avoidable) outcome. If needed however, amputation can of course lead to another form of reconstruction – with modern artificial limbs (prostheses).
Further information on the diagnosis and treatment options for PVD is available at the time of consultation with one of our specialist vascular surgeons.